Understanding Primary Periodic Paralysis (PPP) to pave a path forward
PPP is a rare genetic disorder that causes episodes of muscle weakness and temporary paralysis.1 The information and resources on this site may help you learn more about PPP including how it’s managed and how it’s diagnosed.

Find a doctor who diagnoses and treats PPP

Learn more about a treatment option for PPP

Hear real-life PPP experiences
PPP can be triggered by certain aspects of your lifestyle
Triggers of PPP can vary from person to person and from one type of PPP to another, but some common ones include1,2:
- Foods or beverages that are high in salt, carbohydrates, or potassium
- Stress or fatigue
- Exposure to cold temperatures or cold air
- Rest after exercise
You can work with your doctor to understand what your triggers for PPP are, how to avoid them, and to determine a treatment plan that works for you.
Take control of your PPP with the right choices and the right treatment option1
PPP can impact your daily life, but it can be managed with lifestyle changes to avoid triggers and with treatment.1
It’s important to understand that PPP can have long-term consequences2,4
After a number of years, PPP may lead to Permanent Muscle Weakness (PMW).2,4 This is weakness that does not go away and isn't associated with any specific episode. After suffering from PPP episodes for years, you may experience muscle loss.4 PMW can limit your ability to move, impacting your work, family, and social life.4 Ask your doctor for more information about PMW.
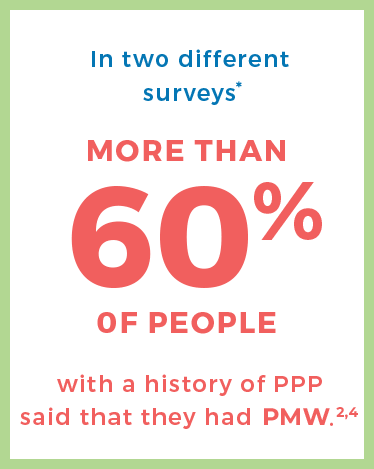
*One survey included 66 self-selected patients over the age of 40 who were diagnosed with PPP who sought support through the Internet; the other survey was of 137 patients with a median age of 46 years who were diagnosed with hyperkalemic periodic paralysis (HyperPP) and were invited through the Internet or a healthcare institution to participate.2,4
Learn more about treatment for PPP.
Wherever you are in your PPP journey, these resources may help
Be Your Family Facilitator brochure & family history worksheet
The family facilitator brochure will help you get ready to talk with your family about PPP, and why it's important to get diagnosed and manage the condition if they also have PPP. The family history worksheet will help you map out the pattern of PPP in your family.

PPP white papers
These white papers were developed by doctors with experience diagnosing and treating PPP. They cover some common methods to help physicians and patients better understand these challenges with PPP.
30% of patients do not have one of the gene mutations known to cause PPP.1 Discover other ways it can be diagnosed.
Sign up to receive PPP educational materials and resources
All fields required unless otherwise noted.
Frequently Asked Questions (FAQs) About PPP
PPP is a rare genetic condition that can cause episodes of muscle weakness or temporary paralysis. Episodes are often triggered by certain aspects of a person’s lifestyle or diet. There are several sub-types of PPP including: hyperkalemic, hypokalemic, paramyotonia congenita, and Andersen-Tawil syndrome.1 In the United States, only about 4,000 to 5,000 people have been diagnosed with PPP.3
There is more than one type of PPP and the estimated number of people that have each type varies
Hyperkalemic (approximately 1 in 200,000)1
Some of the common features include weakness in the arms and/or legs and high potassium levels in the blood. Sometimes potassium levels can remain normal.
Hypokalemic (approximately 1 in 100,000)1
Some of the common symptoms include muscle weakness that can last for at least several hours and low potassium levels in the blood.
Paramyotonia congenita (approximately 1 in 100,000)2,5
A common symptom is constant muscle tensing that prevents muscles from relaxing. Potassium levels in the blood can be high or normal.
Andersen-Tawil syndrome (approximately 1 in 1 million)1
Some of the common symptoms include unusual physical features of the skeleton and unusual signs when the heart is monitored. Potassium levels in the blood can be low, high, or normal.
All of these types of PPP cause muscle weakness and/or stiffness that can impact several parts of the body.1,5
PPP is a genetic condition, and children have a 50% chance of developing the disorder if one of their parents carries a gene for PPP. This is called "autosomal dominant."1
Reported during attacks:
- Muscle weakness, with or without the feeling that you can't unclench your muscles (called myotonia)2,5
- This weakness usually lasts several hours and can resolve spontaneously2,6
- Shifts in potassium levels2,6
Reported after attacks2:
- Clumsiness
- Extreme fatigue
- Weakness
- Muscle pain
The burden of PPP episodes is not only physical
Weakness, loss of energy, and stiff muscles can limit people's ability to participate in activities including social and family life, sports, and even school and work.2,4
Anxiety can also be a problem. People living with PPP often fear an impending episode and are worried about how others may look at them or pity them during an episode. This can lead to a cycle of continued stress, which can trigger an episode, which can lead to stress, and so on.2
PMW is a common long-term consequence of PPP2,4
PPP may lead to progressive Permanent Muscle Weakness. This is weakness that does not go away and isn't associated with any specific episode.2,4 After suffering from PPP episodes for years, some people may experience muscle loss.4 Permanent Muscle Weakness can limit the ability to move, impacting work, family, and social life.4
IN TWO DIFFERENT SURVEYS, MORE THAN 60% OF PEOPLE WITH A HISTORY OF PPP SAID THAT THEY HAD PERMANENT MUSCLE WEAKNESS.*2,4
*One survey included 66 self-selected patients over the age of 40 who were diagnosed with PPP who sought support through the Internet; the other survey was of 137 patients with a median age of 46 years who were diagnosed with HyperPP and were invited through the Internet or a healthcare institution to participate.2,4
Diagnosis can take up to 20 years2
Unlike some medical conditions where a simple blood test can determine the source of symptoms, PPP can be extremely difficult to diagnose, taking up to 20 years in some cases, and it can also be misdiagnosed.2 Many people with PPP have reported being misdiagnosed with other conditions, including conversion disorder, mental disorders, and depression, before receiving their diagnosis.2
In order to make a diagnosis of PPP, your doctor will usually review your medical history and your family medical history, then perform a physical exam and run a genetic test if PPP is suspected. If the test results come back positive, then a diagnosis can be confirmed. If the test results come back negative, your doctor may perform blood tests or other tests.1
Looking for a doctor who has experience diagnosing PPP? Start searching
Tests that help diagnose PPP
Genetic
This type of test involves collecting a sample of an individual's saliva or blood to look at the DNA.7 The reason this is done is because PPP is a genetic disorder.1 Genetic tests look for specific gene mutations that have been identified and determined to cause the different subtypes of PPP.1,7
ECG/EKG
An ECG or EKG, short for electrocardiogram (ee-LEK-tro-CAR-dee-oh-GRAM), is used to detect abnormalities in the heart’s rhythm.8
EMG
Short for electromyography (ee-LEK-tro-my-AH-grah-fee), EMG is used to record the electrical activity of the muscles to see if they contract and relax properly.9
CMAP
Compound muscle action potential, or CMAP, is also known as an exercise EMG and is used to record changes in muscle function and nerve activity after spreading the fingers (or raising the toes) against resistance.1
Looking for a doctor who has experience diagnosing PPP? Start searching
There is a treatment option that has been shown to reduce the number, severity, and duration of Primary Periodic Paralysis attacks in two (2) separate clinical studies. However, not every patient has the same response to treatment.10 It also helps to avoid any foods or activities that trigger episodes of PPP.1
In addition to lifestyle adjustments, PPP is managed with treatments that work to control episodes.1 There is currently only one FDA-approved treatment for PPP.
Learn more about this treatment
Understanding PPP helps you have an informed conversation with your doctor about how to manage it.
Identifying and avoiding triggers is critical
- Record the triggers that caused an episode
- Work with your doctor to develop a plan to avoid triggers
- Remember that triggers are different for everyone, and the lifestyle modifications that work for one person may not work for another
Learn more about treatment for PPP.